Why adding an ultrasound-guided erector spinae plane (ESP) block to the standard enhanced recovery protocol is a game-changer for patients following surgery.

In an article published in the March 2022 issue of Anesthesiology News, titled, Post-op Opioid Use Less With ESP Block in Lumbar Open Fusion, writer Michael Vlessides speaks with Integrated Anesthesia Associates (IAA’s) Theresa Bowling, MD, and examines the evidence of how this trailblazing team’s strategic application of local anesthetic through an ESP block has proven to provide an impressively significant reduction in the need for pain medication during the first three days of recovery. (View full article below)
“It’s an honor to have our team’s research presented as a feature story in AN, a publication I have been reading since I was a resident”, Dr. Bowling stated. “Having our study featured in Anesthesiology News (AN) makes our data easily accessible to over 50,000 subscribers. Readers can review our data from other perspectives, with the potential of offering new insights from the original work.”
Theresa Bowling, MD
Director of Anesthesia Connecticut Orthopaedic Institute
& Ayer Neuroscience Institute at St.Vincent’s Medical Center
IAA couldn’t be prouder of Dr. Bowling for this outstanding achievement, and her team’s ongoing success in improving clinical outcomes and positively affecting patients’ lives through innovative research and protocols. Please join us in congratulating Dr. Bowling and the entire research team for this exceptional work which is gaining well-deserved attention and consideration. We welcome your comments and feedback as well.
A recent reader wrote the following in response to the article posted below:
“Dear Dr. Bowling,
….I really would like to speak with you and network. Our experience with ambulatory spine led to our development of equally impressive ERAS protocols for ambulatory arthroplasty. Congrats on being a trailblazer. It appears you have the same passion for the rightful role of the anesthesiologist as the perioperativist. I am teaching the next generation of anesthesiologists now but have a keen interest in disruptive innovations allowing a continued shift or in patient-to-outpatient procedures in specialty centers. It’s loads of fun.”
W.W., MD
LEARN MORE:
Physician Bios and Centers
Robert Suriani, MD, FASA, FASE
The Connecticut Orthopaedic Institute at St. Vincent’s Medical Center (COI)South
The Ayer Neuroscience Institute at St. Vincent’s Medical Center
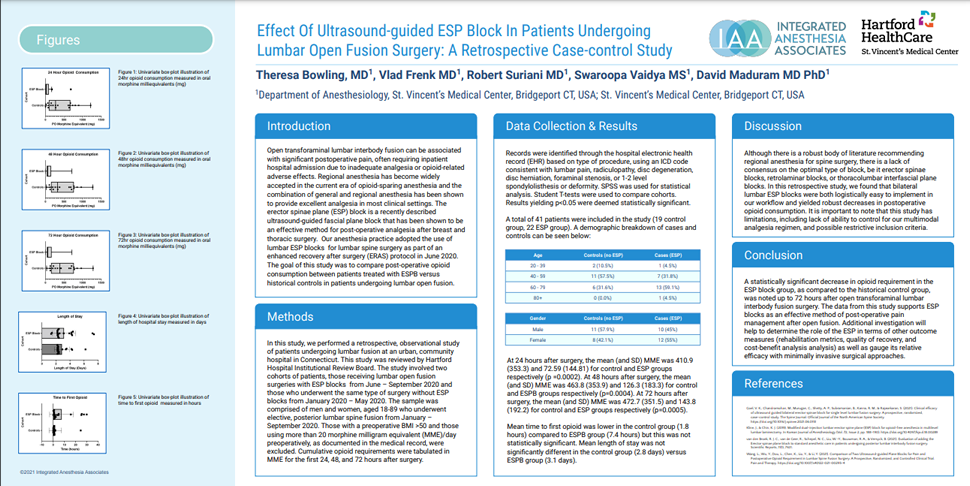
The Research Retrospective Case-control Study:
Bowling, T., Frenk, V., Suriani, R., Vaidya, S., Maduram, D. (2021)
Effect Of Ultrasound-guided ESP Block In Patients Undergoing Lumbar Open Fusion Surgery: A Retrospective Case-control Study.
American Society of Anesthesiology Annual Meeting, San Diego CA, October 8-12, 2021
Download the PDF
View other anesthesia research from this IAA team
The following has been reprinted with permission from Anesthesiology News
View the original article here:
MARCH 16, 2022
Post-op Opioid Use Less With ESP Block in Lumbar Open Fusion
San Diego—Regional anesthesiologists can add lumbar open fusion surgery to the list of procedures in which the erector spinae plane (ESP) block can play a beneficial part.
A team of Connecticut researchers found by adding the ultrasound-guided ESP block to an existing enhanced recovery after surgery (ERAS) protocol, they were able to significantly decrease postoperative opioid requirements for up to 72 hours in these procedures.
“Although there are pilot studies and case reports on the safety and efficacy of the erector spinae plane block in lumbar surgery, there’s a general paucity of studies,” said Theresa Bowling, MD, the director of anesthesia for the Connecticut Orthopaedic Institute, in Meriden, and the Ayer Neuroscience Institute at St. Vincent’s Medical Center, in Bridgeport, Conn. “Having recently incorporated the block into our ERAS protocol for lumbar spinal fusions and observing the profound impact on decreasing narcotic consumption for pain management, we decided to review our own institutional data.”
Bowling and her colleagues studied the records of patients 18 to 89 years of age presenting to the institution for nonemergent posterior lumbar spine fusion surgery (Figure 1). Patients were divided into two groups: those who underwent the procedure in January 2020, before ESP blocks were introduced at the institution, and their counterparts who underwent the surgery in July 2020, with the ESP block.

Figure 1. Spinal fusion.
Patient records were identified using an ICD-10 code consistent with level 1-2 spondylolisthesis or deformity, lumbar pain, radiculopathy, disk degeneration, disk herniation, or foraminal stenosis. Individuals with a body mass index greater than 50 kg/m2 and those using more than 20 morphine milligram equivalents (MME) per day, as documented in their medical records, were excluded from the study.
The primary outcome of the analysis was cumulative opioid requirements (expressed in MME) for the first 24, 48, and 72 hours after surgery.
‘A Game Changer’
In a presentation at the 2021 annual meeting of the American Society of Anesthesiologists (abstract A4180), the researchers reviewed data from the 41 patients included in the final analysis, 22 of whom underwent surgery with ESP block (55% female) and 19 of whom did not and served as controls (42% female). They found that at 24 hours after surgery, the mean MME was 72.6 for ESP patients, significantly less than the 410.9 consumed by controls (P<0.01).
Similar differences were found between groups at both 48 and 72 hours. Patients who underwent surgery with the ESP block consumed a mean of 126.3 MME at 48 hours, significantly less than controls who consumed 463.8 MME (P=0.004). At 72 hours postoperatively, ESP patients had consumed 143.8 MME, while controls had used 472.7 MME.
“The ESP block was a game-changer with respect to the decrease in narcotic usage in the postoperative period,” Bowling noted. “We didn’t anticipate the profound impact that ESP blocks would have on decreasing narcotic consumption when we added it to our already successful ERAS protocol.”

Figure 2. Theresa Bowling, MD, reviews planned blocks preoperatively with Robert Brady, MD, spine surgeon.
Perhaps not surprisingly, the mean time to first opioid use was markedly prolonged in patients who underwent fusion surgery with ESP block (7.4 hours) compared with controls (1.8 hours). This difference, Bowling explained, did not reach statistical significance. The mean hospital length of stay (LOS) did not differ significantly between ESP block patients (3.1 days) and controls (2.8 days).
“The two factors primarily affecting LOS for these cases are pain management and output from the incisional drain,” Bowling said in an interview with Anesthesiology News. “Although patients’ pain was no longer an impediment to discharge, the criteria for drain removal was unchanged, which is why the LOS was so similar between groups.”
No adverse events were noted in patients who received the ESP block, but the researchers did observe one unintended consequence in these individuals. “Almost as soon as we added the block to the ERAS protocol, the surgeons noticed increased drain output for the first 24 hours,” Bowling said. “After meeting with the multidisciplinary team, we discovered the patients had so little pain when they arrived to the inpatient unit that the physical therapists were having patients climb stairs on the day of surgery, when historically patients only went from bed to chair on postoperative day 0. So, we instructed our physical therapists to limit the therapy to walks around the unit, despite minimal pain, and that solved the problem.”
Despite such shortcomings, the researchers vigorously endorsed the use of ESP blocks in patients undergoing lumbar open fusion surgeries.
“We’ve had over 600 patients in our ERAS protocol with ESP blocks, and we have proven that fascial plane blocks have a profound positive effect on outcomes,” Bowling concluded. “The block is easy to master and has a low complication rate, so I firmly believe that other practices should make it part of their spine ERAS protocols.”
An ‘Impressive Result’
Jeffrey C. Gadsden, MD, was impressed with the results. “Managing postoperative pain in spine patients can be challenging, and the authors have demonstrated that the thoughtful application of local anesthetic via an ESP block results in a remarkable reduction in the requirement for pain medication over the first three days—a very impressive result,” said Gadsden, the chief of orthopaedic, plastic and regional anesthesiology at Duke University Medical Center, in Durham, N.C.
“The ESP block has been advocated for a wide variety of procedures, generally with good success,” said Gadsden, who is a member of the Anesthesiology News editorial advisory board. “However, the authors’ findings resonate with our own clinical experience showing an outstanding effect for spine surgical patients. The block seems to be, perhaps not surprisingly, particularly well suited for spine procedures. The ESP block is also safe and technically simple to perform, and I strongly agree with Dr. Bowling that this should be part of a multimodal approach to every spine fusion procedure.”
—Michael Vlessides

